Information on wound healing
Being a barrier organ, the skin is particularly exposed to damaging effects of our environment. After injury of this barrier the tissue damage needs to be repaired as quickly as possible and the skin's protective function must be restored. Normal wound healing is of high priority for the organism. Formation of scab is necessary to avoid excessive losses of water and heat through the wound as well as dehydration of the wound. This also provides protection from exogenous influences, infections and mechanical irritation. Under normal circumstances, wound healing takes place smoothly and the barrier function is quickly restored.
Phases of wound healing
Immediately after injury of the skin repair mechanism are starting in order to restore the skin's barrier function as quickly as possible. The entire wound healing process comprises a number of individual phases. A common characteristic is the activation, co-operation, and secretion of different cell types. The inflammation (proliferative) phase is also a cleansing phase. When the wound is healing, the cleaning process predominates.
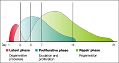
During the latent phase, processes involving the removal of cell debris prevail. Defense against infections and the healing process are starting slowly. In this phase the risk of infection is high. In the subsequent proliferation phase, successful defense against wound infection is most likely due to the formation of new blood vessels in the connective tissue. During that time, all defense mechanisms are mobilized. All overall, this wound healing phase offers the best requirements for a quick, smooth wound repair. About one week after injury, the reparative phase of the healing process begins and the wound closure is starting.
Physiology of wound healing
Wound repair and defense against wound infection require a properly working endogenous defense system. Macrophages are the key cells of the immune system. This Greek word means big eaters
, as they engulf and incorporate pathogens before digesting them. Macrophages are present in all tissues and in the lymph fluid.
On closer inspection of the wound healing, the individual phases of wound healing can be distinguished by their characteristic features. After injury, blood coagulation is activated primarily, and macrophages and granulocytes immigrate. Macrophages cleanse the wound while granulocytes fight against bacteria that have entered the wound. This cleansing/inflammation phase is normally followed by the proliferation phase. New connective tissue is synthesized, vessels emerge into the wound area, and the tissue defect is slowly refilling. Keratinocytes (cells in the epidermis) migrate across the temporary connective tissue and close the defect. Wound closure is followed for some time by rebuilding processes in the connective tissue, which is summarized as cicatrisation phase.
Wound healing disorders and problem wounds
Wound healing disorders are a considerable medical problem. If normal wound healing mechanisms are inhibited by different primary diseases, even a minor injury can result in a poorly healing wound. For an efficient therapy the primary disease needs to be identified and treated, and the pathologically disturbed healing process has to be normalized in a specific way. In rare cases the wound healing process may fail to appear, resulting in a problem wound needing a long treatment period. In fact, there are many diseases that impede normal wound healing. Therefore, patient's primary diseases should always be taken into account in the differential diagnosis of wound healing disorders. Examples of problem wounds include:
- Ulcus cruris (leg ulcers in case of venous insufficiency)
- Decubitus (bedsores or pressure ulcers)
- Diabetic foot ulcers (wounds in case of diabetic neuropathy)
Chronic venous insufficiency is an example of a condition causing local wound healing disorders. By damage of the venous valves the circulatory dynamics in the leg veins are changed, often accompanied with enhanced blood circulation and increase of pressure in the venous vessel system. The final step is the development of venous leg ulcers. Without proper therapy leg ulcers heal very slowly. In this case, the patient's wound healing disorder is limited to the lower legs; other wounds (e.g. following abdominal surgery) often heal smoothly.
Wound treatment with Oxovasin®
The effectiveness of ® solution is based on the stimulation of tissue repair. This has been demonstrated in experiments revealing Oxovasin® to boost phagocytosis (ingestion) and to stimulate the wound macrophages. Oxovasin® activates the wound macrophages in order to enable their key functions in all three phases of wound healing:
- Wound cleansing with defense against infection
- Wound granulation with the formation of new vessels and wound tissue
- Wound closure
Principle of wound treatment with Oxovasin®
Oxovasin® penetrates through the wound and the wound borders into the regenerative tissue layers, stimulates thereabouts the cellular defense, and resolves excessive inflammation reactions in the wound.
Oxovasin® stimulates the macrophages leading to effective defense against infection. Since the wound cleaning processes start from the wound ground, changes to the wound surface need not necessarily be evident at first. The disintegration of necroses (dead tissue) and the simultaneous start of the formation of connective tissue containing plenty of vessels (granulation) are characteristic of wounds treated with Oxovasin®.
Next to wound cleansing and fighting against infections, the stimulation of the macrophages results in the secretion of factors for tissue regeneration and the formation of new vessels. The aqueous solution Oxovasin® supports the humid environment of the wound.
By forming clean, healthy granulation tissue with good blood circulation, Oxovasin® generates the requirements for rapidly visible wound closure with good cicatrisation (scar formation).
Clinical trials demonstrating the efficacy of Oxovasin®
Oxovasin® has been used successfully for more than 30 years for the treatment of badly healing wounds. Its effectiveness has been impressively demonstrated in several clinical trials involving more than 8,000 documented cases. Among others, the efficacy of Oxovasin® was demonstrated in clinical trial conducted 1986 at a number of German hospitals. The results of this study were published in the famous medical journal The Lancet
[1]. The investigator's assessment with respect to wound cleansing, granulation, and the degree of epithelization was statistically significant to highly significant better within the Oxovasin® group (137 patients) compared to the assessment of the patients in the control group (134 patients), who had been treated with physiological saline solution. Moreover, the results of the objective assessment parameters wound contraction (measured using three-dimensional planimetry) and the microbial count in the wound were significantly better in the Oxovasin® group compared to the control group. Other clinical trials have demonstrated the effectiveness of Oxovasin® in connection with severe wound healing disorders that could either not or barely be therapeutically controlled by other wound healing agents available at that time, such as damage to the skin and mucous membrane caused by radiotherapy or chemotherapy.
We are pleased to provide on request additional information to professional interested parties (physicians, pharmacists).